
When it comes to our postpartum bodies, there’s much we don’t discuss. One topic rarely makes the light of day: pelvic organ prolapse (POP).
Yup. After childbirth, our pelvic organs can fall into our vaginal canal and even peek out of our vaginas.
Talking about POP is probably as uncomfortable as having it but it’s an important discussion – especially with female relatives since it can run in the family.
Even without a known family history of prolapse women who’ve had prolonged deliveries, multiple vaginal births, or assisted births with forceps or vacuum are at increased risk. In fact, about a quarter of US women suffer from pelvic floor dysfunction, which includes prolapse.
How does pelvic organ prolapse happen?
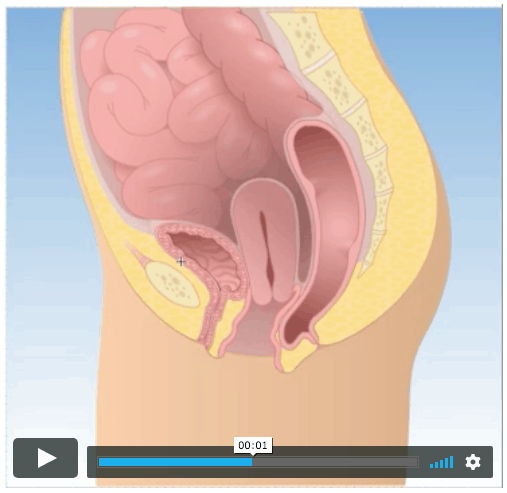
Postpartum hormones. They can weaken the tissue of the vagina and pelvic floor. When the pelvic floor, vaginal wall, abdominal muscles, and ligaments that hold of pelvic organs like the bladder, uterus, rectum and intestines are weak, organs can lean or fall into the vagina. Often, it’s the uterus, bladder or rectum, but sometimes the intestine can prolapse. Click here to see how.
Compromised perineum. The perineum that links the vagina and rectum is a central tendon of the pelvic floor. But women with POP have a compromised perineum. It can feel loose or like there’s a widening, which is common among us who’ve had an episiotomy or vaginal tearing during childbirth.
What are the signs and symptoms of prolapse?
Pressure and heaviness in the vagina are common symptoms of POP. Those sensations tend to worsen throughout the day, particularly if you’ve been on your feet and carrying loads, like a baby.
Other common signs and symptoms of POP include:
- Feeling a bulge vaginally or that something is outside your vagina.
- Difficulty emptying your bladder and/or bowel.
- Urinating twice in one sitting (AKA “double void”). For instance, after you urinate, you change positions or wiggle around to let out more urine.
- Incontinence (stress or urge incontinence).
- Difficulty with bowel movements. Some women may feel their stool through their weakened vaginal wall and need to stick their finger in their vagina to help move along her bowels (AKA a vaginal splint).
Four stages of POP exist:
Stage 1: The uterus or organ is in the upper half of the vagina.
Stage 2: The uterus or organ descends near the opening of the vagina.
Stage 3: The uterus or organ protrudes out of the vagina.
Stage 4: The uterus or organ is outside of the vagina.
Is surgery always necessary for pelvic organ prolapse?
Short answer, no.
Generally, patients in stages one or two who don’t experience symptoms won’t necessarily need surgery. Physical therapy exercises should suffice. But others at stage two sometimes need a pessary—a flexible, removable device—inserted in the vagina to support the vaginal wall.
At stage three or four, you’ll likely need to see a urogynecologist or a colorectal physician. Surgical intervention may be necessary.
How can prolapse be treated?
The first thing is to see a health professional who will take your condition seriously. Too often health providers offer surgery or take a wait-and-see approach for women with prolapse, with little between.
Fortunately, pelvic PTs can treat women with POP, either delaying or preventing surgery. Ask your perinatal
specialist, a girlfriend, or google for leads on pelvic physical therapists in your area. You can also check out the directory from the Herman and Wallace Pelvic Rehabilitation Institute (the industry’s gold standard in the US). For those in Canada, you may want to check out Diane Lee (British Columbia) and Pelvic Health Solutions (Ontario).
How to not make the POP worse (take pressure off your pelvic floor):
Stop lifting heavy things. That means asking people to help load/unload that car, not carrying things up and down the stairs like laundry or even the baby, and opting for the stroller rather than the baby carrier. I know, all these are easier said than done. But lifting puts extra pressure on your already compromised pelvic floor.
Avoid weight training exercises. A lot of new moms want to get back to their running, Crossfit, or start an exercise program to help lose that baby weight. Listen to your body. If you have any symptoms of POP, stop. High impact activities put a lot of pressure on your pelvic floor and can exacerbate symptoms. If you must exercise, try swimming.
Change your pooping mechanics. Straining to go number two puts a lot of pressure on your pelvic floor. Squatting is more ergonomic than sitting on a toilet and can ease some of that pressure. When going to the bathroom, consider putting your feet up on a stack of books or using a Squatty Potty to replicate the squatting position.
Coordinate your abs and pelvic floor with your breathing. When we inhale, our bellies should expand and pelvic floor should relax. On exhale, our transverse abdominis (our deepest abdominal muscle) should engage along with lifting our pelvic floor.
Avoid standing all day. And sit when you feel vaginal pressure or heaviness.
Get help with posture, pelvic floor and core strength. Pelvic PT are most ideal since they can also assess the stage of your prolapse and address more nuanced pelvic floor issues. If one isn’t accessible, there are also programs designed or vetted by pelvic PTs like MUTU, Mommy Berries, and POP UP to help postpartum women with posture, alignment, core and pelvic floor strength.
Whether you suspect you have POP or have stage four prolapse, don’t suffer in silence. Treatment is available. Among all the “new normals” for postpartum women, pelvic organs falling into your vagina shouldn’t be one of them!




Leave a Comment