When I was pregnant with my first child, I left my initial prenatal visit with a giant folder stuffed full of pamphlets, information sheets, charts, FAQ pages, appointment schedules, and breast pump diagrams that were as foreign to me as the Hubble telescope.
I tucked the folder under my arm, thanked my nurse, and dutifully laid everything out on my kitchen table when I got home. Seeing it all — however many pages of things to know, things to do, things to avoid, things to plan and things to think about — was… a bit much. I thought: well, sh*t, this is some nice, light reading.
I read through everything — because I’m a huge nerd and an overeager rule follower going way back to my childhood days of bossing around my younger siblings — and then I kept reading. I read practically everything I could, and it was both way too much and utterly not enough.
We learn these things when we’re pregnant about what we’re supposed to do, what’s best, and what’s not, but I wanted to know why any of it mattered.
I’m trained in the history of medicine, and like any good (ex-)academic, I’m a skeptic at heart. Why, I wondered, did my grandma’s doctor tell her to gain 15 pounds tops while mine is telling me to gain 25? Why do I need a dating ultrasound if I already know when I became pregnant? Why should I bother to make a birth plan?
The more I sought answers to my many, many questions about where, when, and why so much of the pregnancy advice we generally accept as Dogma originated, the more I found myself sinking into quicksand.
My book Carrying On dives headfirst into that morass, but I’ll tell you what I realized in the end: most of it’s not as black-and-white as we think.
Take weight gain guidelines, for instance.
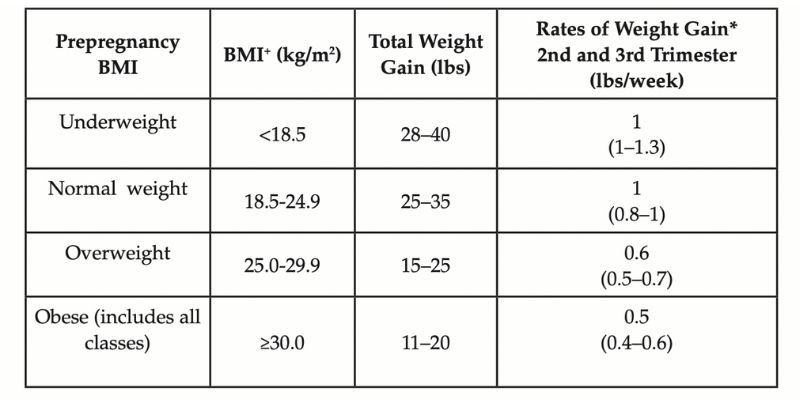
American women today learn to gain X number of pounds depending on their pre-pregnancy body mass index (BMI itself being a subjective form of measurement we could call into question, but we’ll save that for another day), according to the Institute of Medicine’s updated 2009 guidelines:
But medicine’s ideas about what constitutes “ideal pregnancy weight gain” have vacillated back and forth over previous decades. And if we want to really zoom out, we should note that gestational weight gain has only been a “thing” in modern times — scales weren’t even invented until the late 1800s.
Yes, you would likely have received different advice depending on when you became pregnant. There were a few inflection points, and here are the main spans:
Early 1900s:
Who knows? Prenatal care was still in its infancy, and doctors didn’t regularly counsel pregnant women about weight gain using numbers during these years.
Instead, women heard advice like this: "Be not persuaded to humor and feed your appetite’s waywardness; eat with cheer; drink your milk; chew your food to a pulp; and don’t eat very much!: “Enough for one is too much for two.”
So that’s all helpful.

1920s — 1960s:
Most doctors advised pregnant women to keep their weight gain under 15 pounds (!!), partly because they thought this would lead to smaller babies and easier deliveries, but also “to preserve the woman’s figure.” [Facepalm.] If necessary, diet pills were seen as a helpful tactic here.
(If you can’t keep it at 15 pounds, they said, okay, okay, FINE — but you really do need to limit it to 18.)

1970s — 1980s:
New data and analyses led to a completely fresh take, evinced by a National Research Council report: pregnant women should not starve themselves, but rather should “eat to appetite.” And hey! Weight gain ~20-25 pounds is A-okay.
The American College of Obstetricians and Gynecologists even gave the green light to 30 pounds. Clearly, this was a far cry from the previous line of messaging.
1990 — 2009:
The Institute of Medicine devised an individualized set of guidelines recommending weight gain between 15 and 35 pounds, depending on personal BMI.
Almost immediately, critics harangued the IOM guidelines for being way too liberal, saying that they were “encouraging overnourishment,” “encouraging millions of women to overeat,” and “feeding the current epidemic of obesity.” (I remember identifying with a woman who wrote in an article that her first thought when she learned she was pregnant was, “Oh my gosh, I can finally eat a banana.” A banana.)

2009 — present:
Partly in response to criticisms, the IOM further specified weight gain for each BMI group, and in particular set more strict weight gain limits for women with a BMI over 30.
Clearly, each of these “eras” has partly arisen as backlash against earlier ideas — but the echoes reverberate.
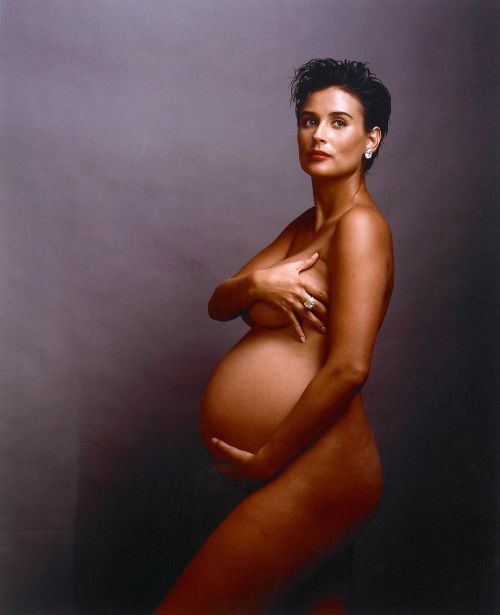
I see two intriguing commonalities across these perspectives: 1) the idea that pregnant women’s appetites and physical bodies need to be controlled; and 2) deviance. While the guidelines have always held some sway and shaped cultural norms (see my pun there?), they have not been gospel. Some women have adhered to the guidelines; some haven’t. Actually, today, most don’t.
Which begs the question — why do we even have them?
Granted, there is some evidence that weight gain far outside the IOM’s recent guidelines — in either direction — is associated with adverse outcomes for moms and babies, but there may also be a reason to believe that pregnancy weight gain may matter very little.
The unsatisfying conclusion? We still don’t entirely know.
Which is fine, right? Well, sort of. Maybe it would be fine if we knew the whole story, but given that the weigh-in is a centerpiece of hospital-based prenatal visits (many midwifery practices eschew the ritual altogether…), and many women are indeed very concerned about tracking their prenatal weight gain, shouldn’t it really mean something?
I like to think so.
Of course, weight gain isn’t the only issue like this — there are so, so many more. The general structure of prenatal care in this country may have changed very little since its inception more than 120 years ago, but The Pregnancy Rules have swelled to the point of being downright labyrinthine.
If you’re interested in trying to get to the bottom of “rules'' such as this, I invite you to check out my book, Carrying On: Another School of Thought on Pregnancy and Health. The book reconsiders much of what we expect and assume about prenatal health and maternity care — without being didactic, prescriptive, or patronizing.
It unpacks the evolution of practices, policies, and norms surrounding nine specific topics central to prenatal care, including the history of managing morning sickness, the rapid expansion of obstetric ultrasound, the haphazard formulation of prenatal exercise guidelines, and the emergence of birth plans. With one foot in the past and the other in the present, the book explores how and why we treat pregnancy — and pregnant women — the way we do.
Also check out: When Did Women Start Lying Down to Give Birth?




Leave a Comment